Healthcare organizations are looking for new ways to address mental and behavioral health challenges to improve clinical outcomes and better manage total healthcare costs—a need that has been exacerbated by the COVID-19 pandemic.
According to a 2021 study from the Kaiser Family Foundation, approximately four in ten adults nationwide have reported symptoms of anxiety or depressive disorder during the pandemic, a four-fold increase from pre-pandemic levels.
At the same time, employees’ expectations for mental health services are increasing. In a 2021 Workplace Wellness Survey by the Employee Benefit Research Institute (EBRI), nearly half of employees reported that mental health wellness programs are more important than before the pandemic, but only 32% said their employer health plan offers mental health resources.
Responding to this rising demand for mental health services is a major priority for healthcare payers, employers, and providers alike. And with good reason—unaddressed behavioral health issues are linked to a loss of productivity, absenteeism, higher levels of disability, substance abuse, and a higher risk of chronic conditions.
One big question for employers and healthcare organizations is how to optimize clinical resources to maximize the impact on costs and outcomes.
Below are three ways some of the most innovative healthcare organizations are leveraging AI and predictive insights to supercharge their mental and behavioral health strategies.
1. Addressing Disparities in Mental Healthcare Access
According to the National Institutes of Health, one in five American adults struggles with mental illness. Perhaps even more devastating is that less than half receive treatment.
Healthcare organizations are looking for innovative ways to address obstacles to accessing mental health resources, whether it be better educating members to existing wellness or therapeutic programs or expanding initiatives such as virtual care and telehealth.
In 2022, more than 100 large employers plan to expand mental healthcare benefits. This year also marks the first that a majority of employers plan to have an anti-stigma mental health campaign.
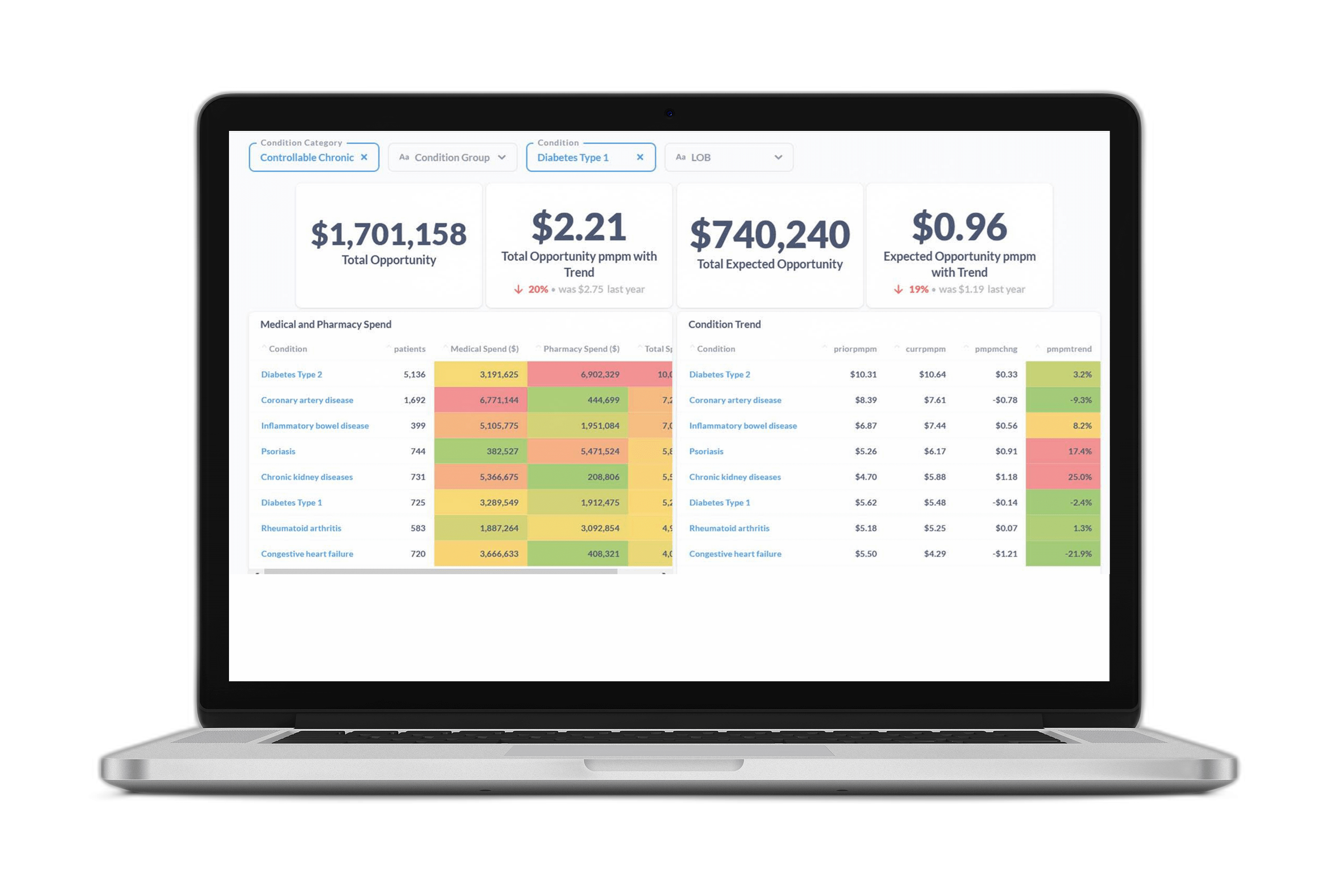
A key component of these efforts is gaining insight into utilization trends for existing programs, the most effective intervention strategies for reaching individual patients, and the risk of mental illness such as depression and anxiety within a population or workforce.
Using an advanced data warehousing and predictive analytics platform, medical management and benefit teams can attain these insights and leverage them to locate pockets of risk, understand which programs are being under-utilized or over-utilized, and pinpoint where new resources are not only needed but would have the greatest impact.
2. Delivering Personalized Outreach and Care
When left untreated, mental and emotional health issues lead to higher levels of disability, lost work productivity, job loss, and employment changes, according to the World Health Organization. Poor mental health is also a risk factor for substance abuse as well as chronic conditions such as diabetes, asthma, cancer, cardiovascular disease, and arthritis.
As a result, there is no standard indicator of a potential issue. The risk factors can be dispersed across many data sources, and across both the medical and pharmacy benefits. Using traditional retrospective tools that are unable to connect dots across multiple data feeds often leaves payers reacting to mental illnesses rather than helping prevent and treat them.
That’s why healthcare organizations are leveraging advanced data warehousing and predictive model solutions to connect all of their health and benefits data, enabling them to understand the true level of risk for a range of mental health issues within their population.
With advanced data warehousing and AI-powered predictive models, healthcare organizations are able to make proactive, data-driven decisions that guide patients and employees to preventative programs tailored to their needs–before an adverse event occurs.
The result is personalized care delivery strategies that match the right member to the right resource at the right time.
3. Evaluate Behavioral Health Program Performance
Evaluating the results of clinical programs is crucial to ensuring the investment is worthwhile, but traditional analytic tools that don’t connect all health and benefits data can leave payers blind to which programs are being used and having a positive impact on outcomes and total cost.
Each program is unique, with different objectives and ways of measuring success. An increase in utilization rates may meet one program’s goals, while an increase in medication adherence could signal another investment is successfully closing a gap in care.
Health plan and employer teams need real-time, wide-angle views of an array of metrics to understand what may be driving changes in utilization rates, measure feedback, and pinpoint where additional resources may be needed.
Using a predictive analytics and data warehousing platform, healthcare organizations are equipped with real-time updates on how their programs are performing. This enables them to transparently communicate their success to internal stakeholders, and successfully build business cases to expand an existing program or invest in new resources.
Learn more about how Certilytics helps healthcare organizations, employers, and other plan sponsors make smarter business decisions, faster. Email contact@certilytics.com to schedule a free consultation with our team of experts.