Discover Opportunities. Prioritize At Risk Populations.
Shift to building programs based on who are your most at-risk populations through the enrichment of your data using a library of 1,000+ clinical, financial and behavioral predictive risk scores to identify future risks and clinical and financial opportunities.
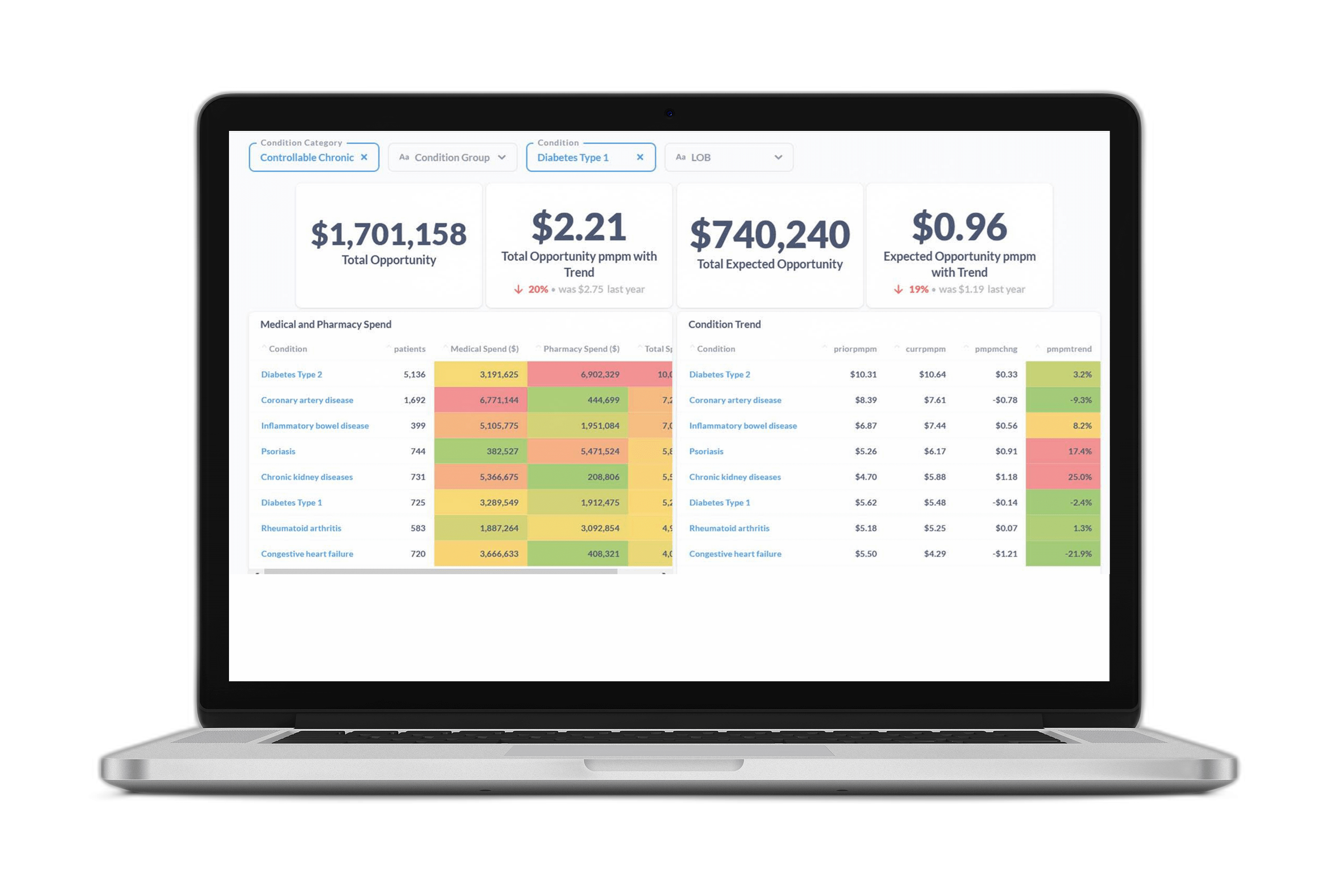
Quickly characterize the health of your population by tracking gaps in care and understanding condition prevalence and the associated costs and trends.
Aggregate member level opportunities up to the population level using the Opportunity Analyzer and see in dollars the impact of executing different clinical programs based on outcomes or disease state.
Be confident your clinical program outreach strategies are reaching those members who are most likely to modify their behavior and improve their health using Certilytics’ member-level Target Index. This approach allows you to maximize your outreach and streamline operational and clinical resource efficiency.