Healthcare organizations must differentiate themselves through their ability to make data-driven decisions that maximize provider efficiency, improve member health, manage costs, and demonstrate value.
Passive data vendors and commoditized analytics do not provide the insights needed when making those decisions. Instead, the most innovative organizations are working with sophisticated data partners that play an active role in driving better decisions about where to direct health management dollars and how best to allocate clinical and digital resources. These organizations are looking forward, and are focused on connecting members with high-value providers to drive meaningful behavior change that improves health and reduces costs.
Below are five questions to consider when selecting your next data partner:
1) Can you unify clinical and financial insights?
We’ve seen firsthand how clinicians and actuaries often work off different data sets and models to evaluate and manage risk. As payers strive to manage total costs, it’s not enough for your data warehouse to simply link your data – you need to also create a unified, forward-looking set of insights that can inform and align your clinical and financial decisions.
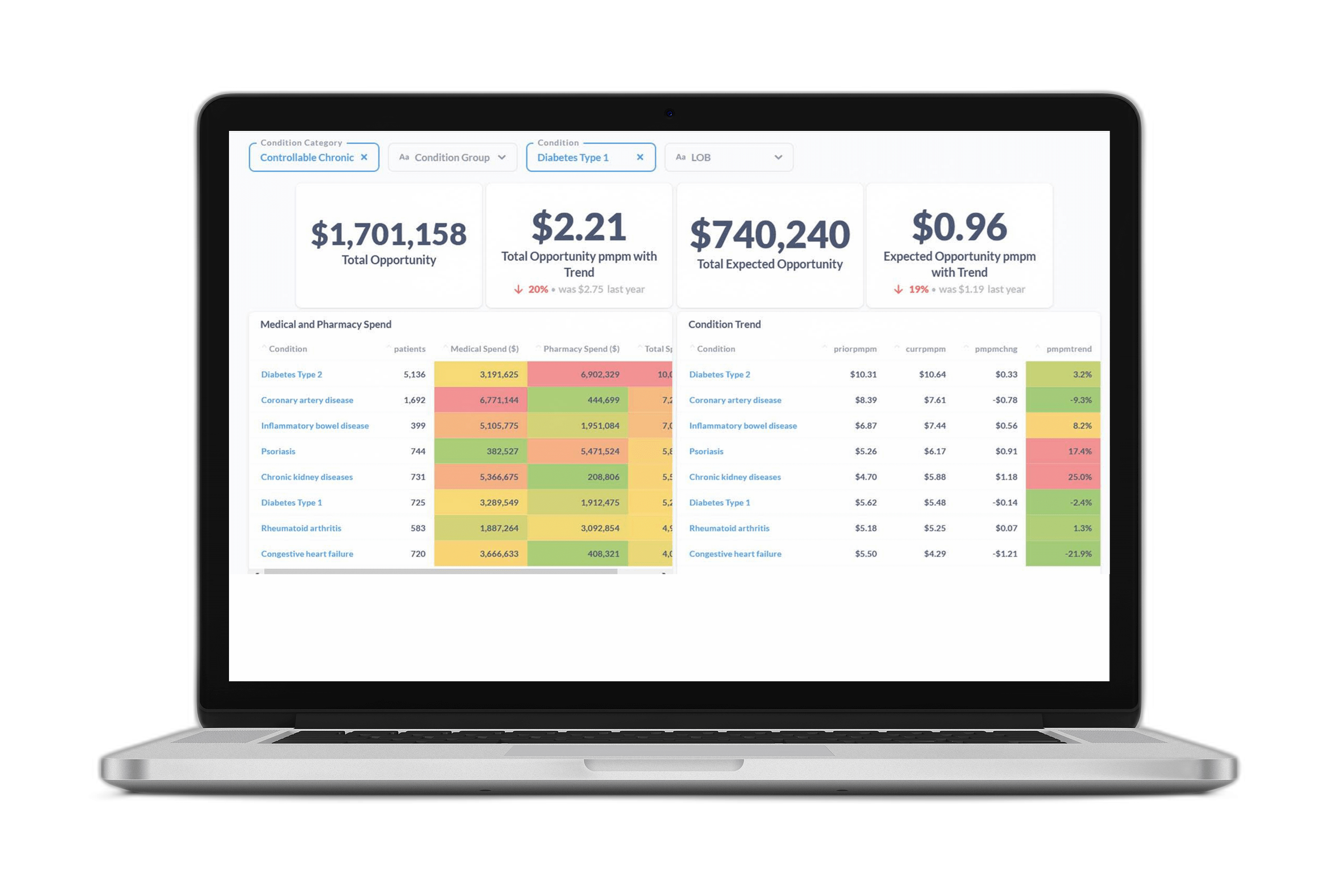
Certilytics’ Opportunity Framework ties clinical outcomes to financial opportunities, aligning stakeholders by showing the value, in dollars, of steering members toward high-value providers, closing gaps in care, enabling earlier interventions for those with emerging chronic conditions, and avoiding high-cost events.
2) Can you integrate medical and pharmaceutical data for cross-benefit analysis?
A traditional data warehouse vendor may share insights about a member’s history utilizing certain benefits. However, to demonstrate value, you must understand how intervention on one benefit (such as drug compliance) impacts other benefits (like medical utilization and avoidance of the ER).
With the CORE® clinical episode grouper, Certilytics integrates pharmacy and medical data to form a complete picture of member health, allowing our customers to “connect the dots” and point to the tangible benefits of their activity on each member’s total healthcare costs.
3) How will you find new and innovative opportunities?
As major cost drivers, high-cost claimants are understandably a top focus of data analytics and many “industry standard” predictive models. However, to manage total healthcare costs, payers must also be able to identify emerging risks to create effective outreach strategies before those members incur exorbitant costs.
Our clinical risk models don’t just look backward at a member’s utilization—but instead look forward at how likely each member is to utilize healthcare services in the future. This includes predicting members who will develop chronic conditions, or who may already have a condition but haven’t yet engaged with the healthcare system—to enable earlier interventions to prevent or better manage these conditions.
4) How will you identify and prioritize the most effective outreach strategies?
Identifying risk is only one component of driving better population health management. Without effective outreach, risk stratification isn’t worth much. In our experience, the most successful outreach strategies rely on more than one method to connect with members. A useful data warehouse vendor will be able to not only identify risk, but also tell you how to reach your members and maximize engagement.
Certilytics solutions can tell you which modalities are most effective, and which members are most likely to engage with a care management plan. Using our engagement model, one national insurer found that members identified as highly likely to engage were 2.6 times likelier to change their behaviors as a result of clinical outreach.
5) How quickly and easily can you measure program performance?
Retrospective evaluation of clinical programs is hard. Few organizations are able to adequately control for confounding factors, particularly when it comes to determining savings across benefits and vendors. Payers need a transparent and timely method for tracking program performance—during and after implementation. Indeed, when multiple third-party managers are vying to take credit for affecting positive outcomes, the vendor with the most timely and understandable performance reporting will win.
With Certilytics, you won’t just save money—you’ll understand exactly why you’re saving money and have the full support of our team of industry experts.