If you’re like most benefit advisors, you’ve made benefit recommendations in the past by aiming for the best discounts and widest networks for your clients.
Each year, you’ve done the hard work of analyzing key performance metrics and worked toward your goals based on data that looked at the past.
But still, you’ve continued to see costs rise with no end in sight. The pressure to contain those costs while delivering benefit recommendations that improve employee well-being only continues to increase.
So, how can you shift from reacting to these high-cost events to being more proactive and preventing them in the first place?
You’ve already got the answers at your fingertips – it’s in the healthcare data. The key to proactive and preventative benefit offerings is utilizing your client’s data to its fullest extent. It’s about leveraging AI to uncover insights that easily show you what’s ahead – before that high-cost event happens.
Keep reading to find how benefit advisors are making the shift to AI-powered benefit design with data analytics that look forward instead of backward.
Choosing the Right Health & Wellness Programs with Forward-Looking Analytics
You’re used to getting reports each year on how your client’s benefit programs performed based on set key performance metrics. Maybe those metrics are how much a program was used, employee survey results, or the prevalence of high-cost events through claims data.
This kind of analysis is traditional and common – a lot of data warehouse and analytic vendors have these reports that use basic, KPI-style metrics that only look in the rearview mirror.
You’ve used these insights to decide where your client should invest to keep their population healthy and manage costs.
Still, unanticipated high-cost events occur, and health and wellness investments go underutilized. In order to better anticipate unique employee needs, more benefit advisors are shifting to AI-based analytics.
What’s the difference?
- All data sources (medical, pharmacy, dental, vision, wellness programs, etc.) are connected on a predictive data and analytics platform to get a holistic view of employees health
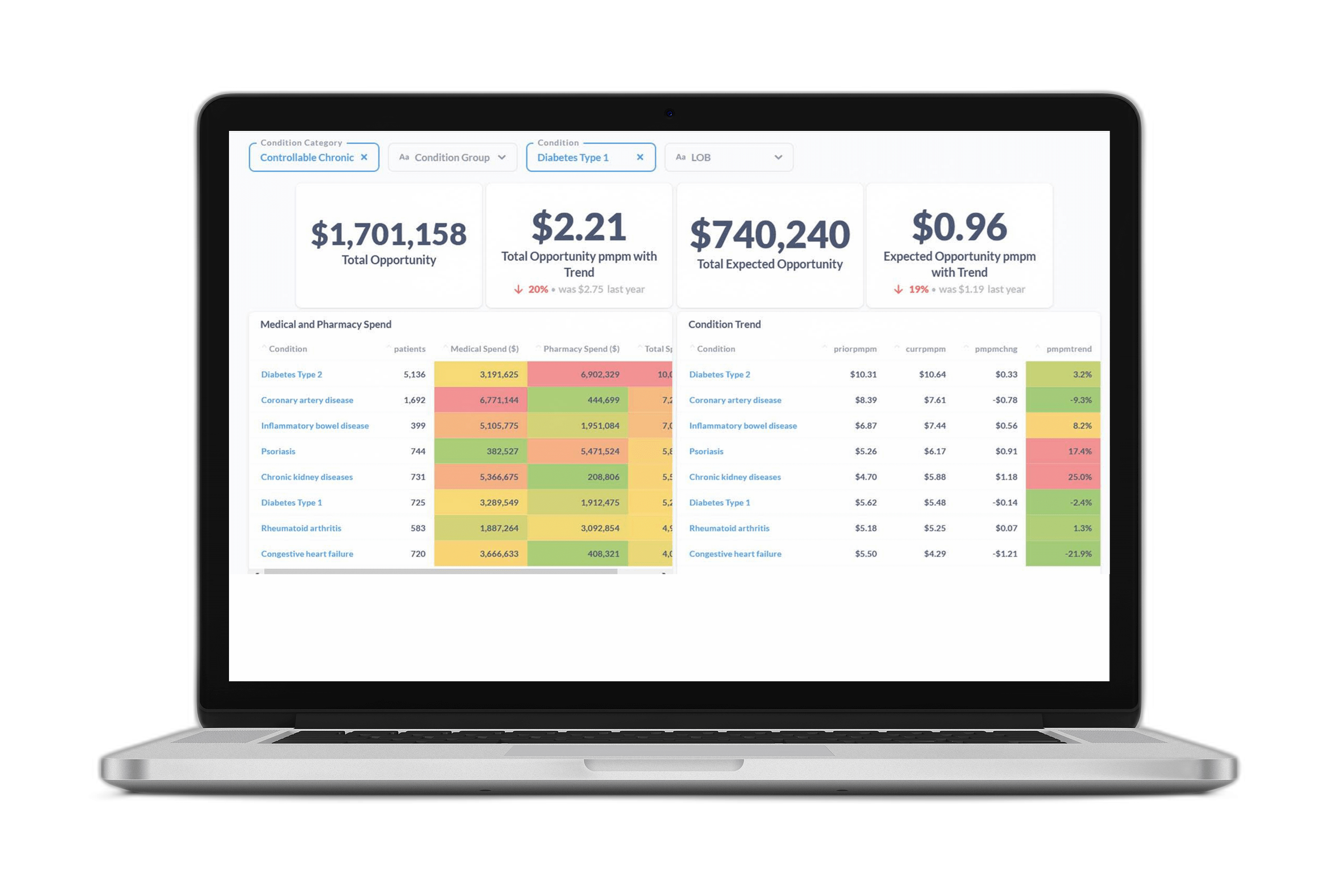
- Benefit advisors can easily see the future prevalence of specific conditions and the avoidable costs on the horizon
- They can test programs as well as point solution vendors to see which will have the biggest impact on health and costs
For instance, heart disease might be the most prevalent and/or costly condition within your client’s population, but the data may show that employees with this condition are already extremely compliant and getting the preventive care they need.
Diabetes may be less prevalent, but the insights tell you there are bigger opportunities for modifying employee outcomes and avoiding high-cost events. With these insights, you could decide to recommend investing limited dollars in a diabetes management program rather than a heart disease program.
An effective, forward-looking analysis allows you to visualize these emerging needs and engagement preferences.
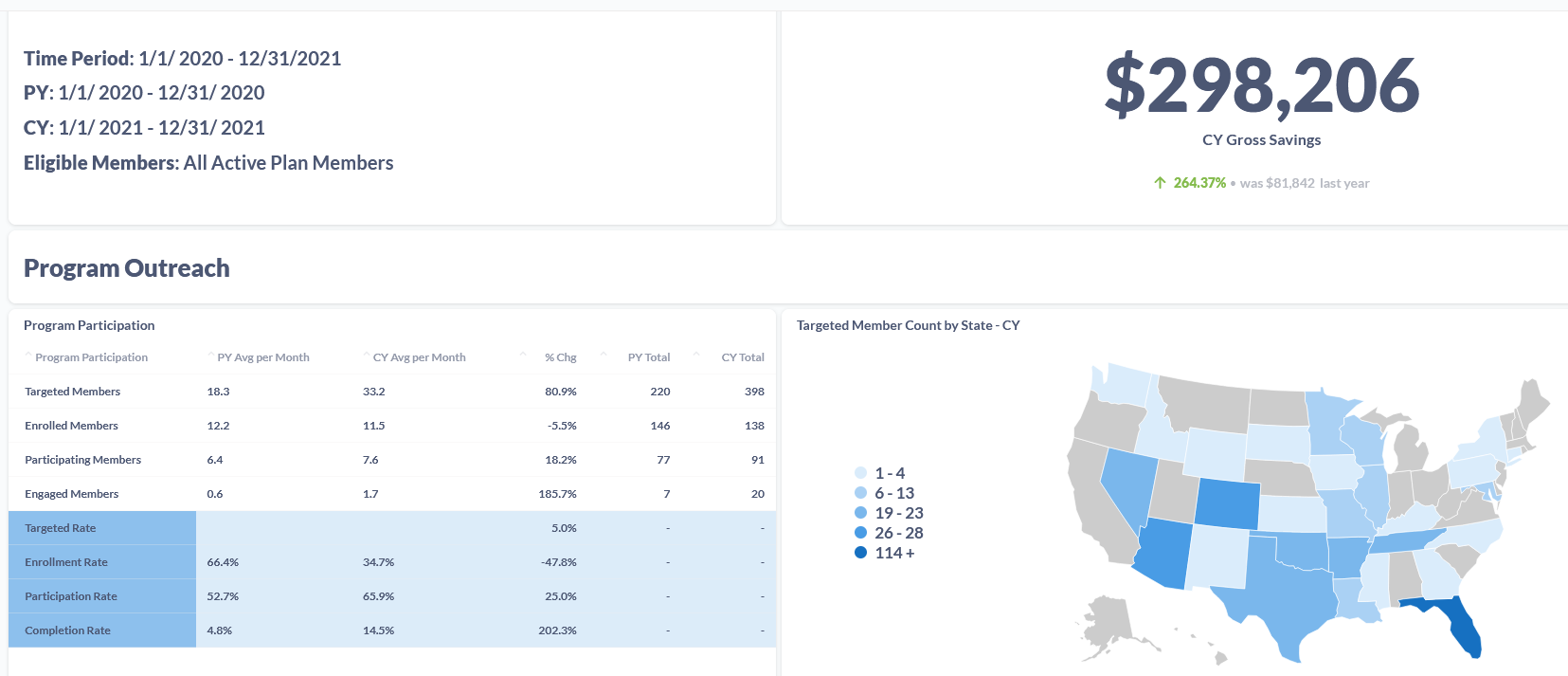
Here’s a snapshot of what information benefits advisors we work with have access to when trying to determine the right solution:
Benefit advisors can see the impact of different benefit plan options and their potential effectiveness as well as cost implications before implementation.
Maximize Your Client’s Program’s Impact with AI-Powered Engagement Metrics
It’s a common frustration we see among HR & Benefit advisors: you identified an issue, helped put a program in place, but then no one used it.
These decisions made sense based off the analytics you received that looked backward. It’s what may have been needed, but those who would benefit didn’t engage with the program.
How can you gain confidence that your health & wellness program recommendations will be used to their fullest potential?
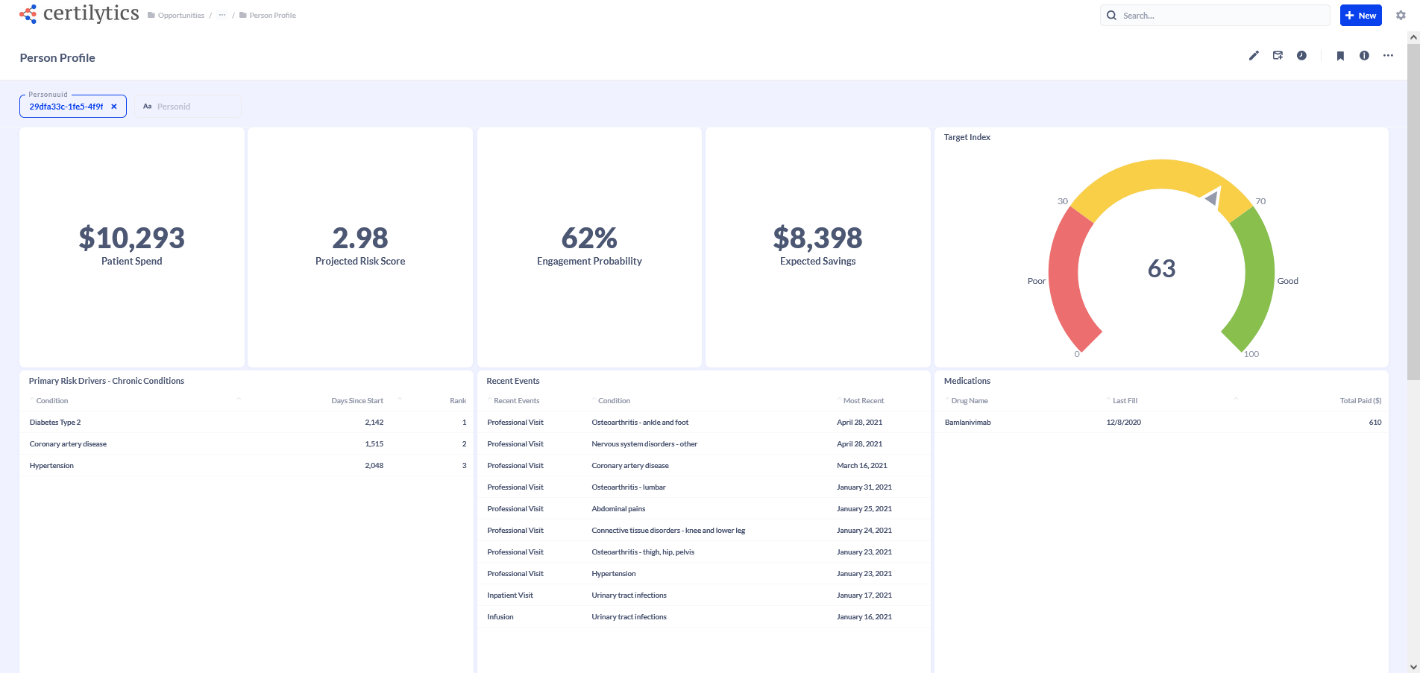
With AI-powered insights, you can measure each employee’s likelihood to engage. As a result, your recommendations will direct outreach and education resources to those employees who are most likely to change their behavior to improve their overall health and well-being.
For example, through Certilytics’ engagement score, you can calculate who is most likely to positively respond to education around taking their prescribed medication, and what’s the potential ROI for getting an employee to take that medication.
Measure a Program’s Success with Data-Backed Insights
You already know how hard it is to measure an internal program’s success or a point solution vendor’s performance.
Most data warehouse and analytic vendors can show you changes in program engagement and cost over time. But when you only look at that year-over-year trend, it’s impossible to determine the actual impact of that program because so many other factors aside from the program also influenced cost.
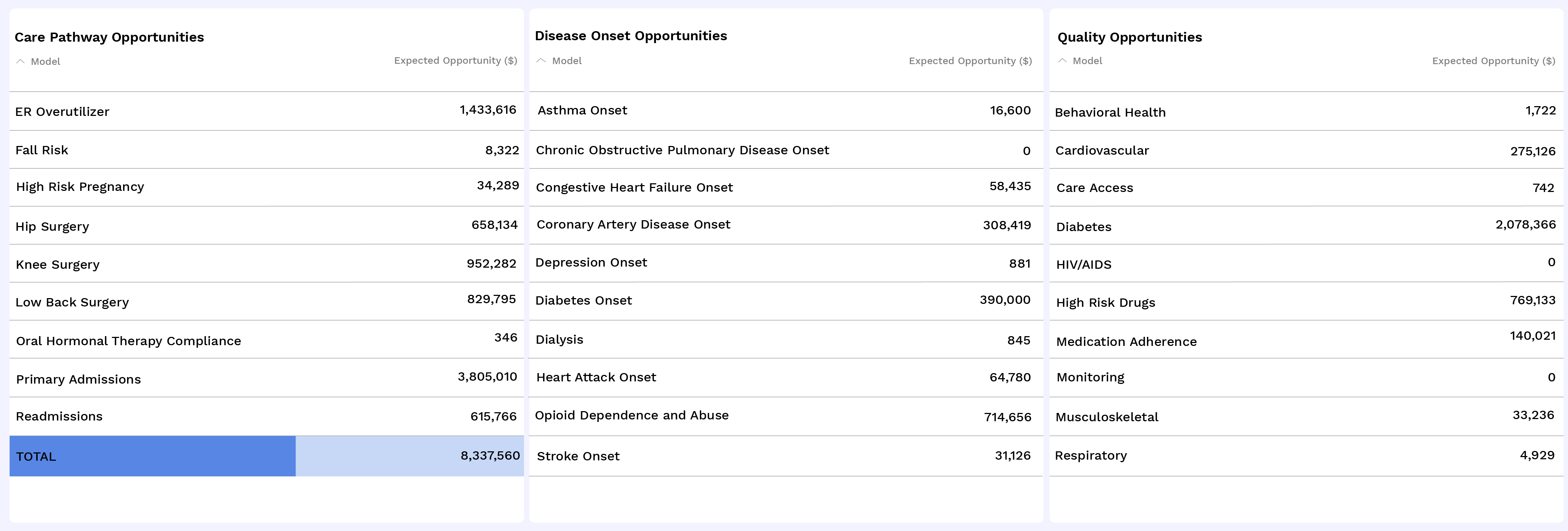
An advanced data and analytics platform can isolate your program’s impact to give a precise picture of that new wellness program’s impact, or the performance of a potential or current solution vendor. You have the actual clinical and financial outcomes at your fingertips.
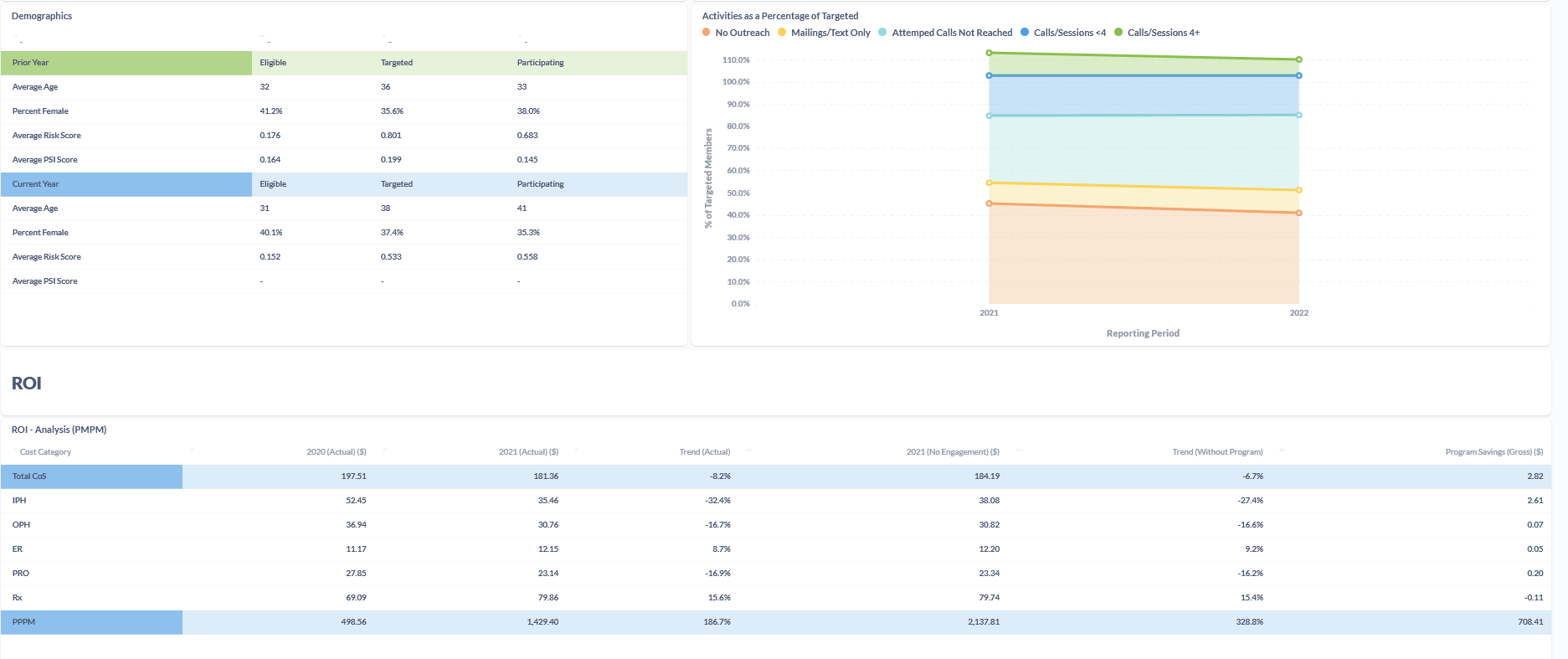
Take a look at the information benefits advisors receive through our Program Performance Analytics Solution for measurement of program success:
Are you ready to shift to AI-powered analytics to address avoidable costs and improve your client’s employees’ health? Schedule a meeting with our team.